Your health is deeply intertwined with understanding how your body functions, especially regarding Type 2 diabetes. It’s a common misconception that your pancreas is the problem when, in fact, the real issue often lies in your body’s response to insulin and lifestyle choices. By uncovering the shocking truths behind what actually causes Type 2 diabetes, you can empower yourself to make better decisions that could improve your overall health and possibly reverse your condition.
Key Takeaways:
- Type 2 diabetes is largely driven by lifestyle factors such as diet and physical activity, rather than a ‘broken’ pancreas.
- Insulin resistance, rather than insulin deficiency, plays a significant role in the development of type 2 diabetes, which can be managed through lifestyle changes.
- Addressing systemic issues such as food quality and accessibility can have a profound impact on diabetes prevention and management.
The Misconception of a “Broken” Pancreas
The idea that your pancreas is “broken” is not only misleading, but it can also mask the true dynamics of Type 2 Diabetes. Instead of viewing it as a malfunctioning organ, consider how lifestyle factors and metabolic processes contribute to insulin resistance. This faulty perception may lead to inappropriate strategies for managing your health, overshadowing the importance of addressing underlying issues such as diet, activity levels, and stress management.
Myth busting: What does it mean to have a ‘broken’ pancreas?
Labeling the pancreas as “broken” simplifies a complex metabolic disorder. In reality, Type 2 Diabetes arises from a combination of insulin resistance, lifestyle choices, and genetic factors. Your pancreas may still produce insulin, but its effectiveness is hampered by factors like obesity or inactivity, demonstrating that it’s not broken, but rather overwhelmed by external influences.
The biological role of the pancreas in metabolism
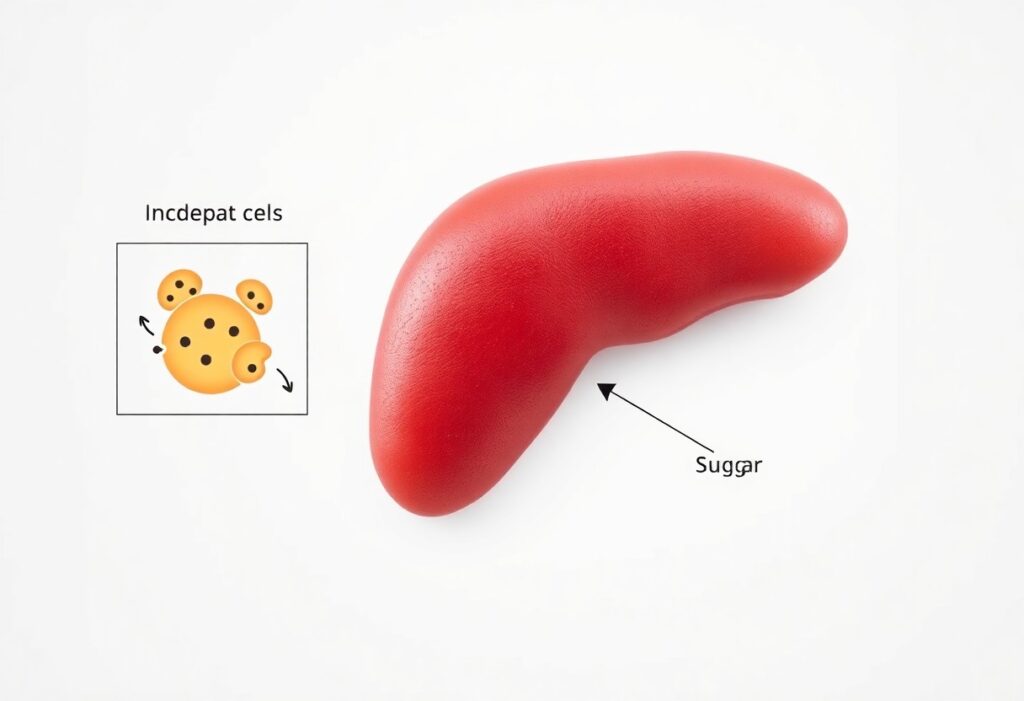
The pancreas plays a vital role in regulating metabolism by producing insulin and glucagon, hormones important for maintaining glucose balance. Insulin facilitates the uptake of glucose into cells for energy, while glucagon prompts the release of glucose when blood sugar levels are low. This finely-tuned process ensures that your body functions smoothly, underscoring the importance of a healthy lifestyle to support pancreatic health and optimize your metabolic response.
Understanding the pancreas’ role is fundamental in grasping how your body responds to food intake. When you consume carbohydrates, your blood glucose levels rise, signaling the pancreas to release insulin. This hormone not only lowers blood sugar by promoting glucose uptake but also helps in fat storage and influences your appetite. If your cells become resistant to insulin due to high fat intake or lack of activity, the pancreas works overtime, leading to potential burnout or dysfunction. Therefore, maintaining a balanced diet and regular exercise can help prevent this overload and support healthy pancreatic function.
The Real Culprits Behind Type 2 Diabetes
Understanding what truly causes type 2 diabetes involves looking beyond the pancreas to uncover a combination of factors. These underlying reasons include genetic predispositions, lifestyle choices, and especially dietary habits. Focusing solely on insulin production oversimplifies the battle against this disease. The interactions between various factors create a complex picture that you must navigate to effectively manage and potentially reverse this condition.
Genetic Predispositions and Lifestyle Factors
Your genetic makeup can influence your susceptibility to type 2 diabetes, but lifestyle choices play a pivotal role in determining your health outcomes. Many people mistakenly believe that high blood sugar is solely hereditary, yet the following factors significantly impact your risk:
- Obesity
- Physical inactivity
- Poor dietary choices
- Stress
Any combination of these factors can elevate your blood sugar levels, leading to insulin resistance and type 2 diabetes.
The Impact of Diet and Nutrition on Insulin Sensitivity
Your food choices directly affect your insulin sensitivity—how effectively your body responds to insulin. Diets rich in whole foods, fiber, and healthy fats enhance insulin sensitivity, while processed foods high in sugars and unhealthy fats contribute to insulin resistance. Research shows that adopting a Mediterranean-style diet, which emphasizes fruits, vegetables, whole grains, and lean protein, can lower blood sugar levels and improve metabolic health.
For example, a study published in the journal *Diabetes Care* found that individuals following a Mediterranean diet had up to a 28% lower risk of developing type 2 diabetes compared to those who consumed more traditional Western diets. Incorporating nutrient-dense foods not only stabilizes blood sugar but also provides important nutrients that improve your overall health. Ultimately, modifying your diet is a powerful tool in managing your insulin sensitivity and reducing the risk of type 2 diabetes.
Insulin Resistance: The Silent Underlying Issue
Insulin resistance often goes unnoticed until it’s too late, quietly laying the groundwork for Type 2 Diabetes. Your body’s cells gradually become less responsive to insulin, the hormone responsible for ushering glucose from your bloodstream into your cells for energy. As a result, your pancreas compensates by producing more insulin, which can lead to an increase in blood glucose levels and, ultimately, diabetes. Understanding this process is vital for maintaining your health.
How insulin resistance develops
Insulin resistance typically develops due to a combination of factors, including poor diet, physical inactivity, and genetic predisposition. A diet high in processed sugars and unhealthy fats contributes to the accumulation of fat, particularly around your abdomen, which is a significant risk factor. This excess fat releases inflammatory substances that interfere with insulin signaling, leading to a cycle of dysfunction.
The role of inflammation and gut health in diabetes
Chronic inflammation and poor gut health play significant roles in the development of insulin resistance. Inflammation caused by a diet rich in refined carbohydrates and artificial additives can disrupt your metabolic processes, making it difficult for insulin to effectively manage blood sugar levels. Moreover, an imbalanced gut microbiome, influenced by factors like diet and antibiotics, can also contribute to insulin resistance and inflammation, exacerbating your risk for Type 2 Diabetes.
Research shows that gut health directly affects insulin sensitivity; a diverse microbiome can promote metabolic health while an unhealthy gut flora may lead to systemic inflammation and impaired insulin action. In fact, studies indicate that individuals with Type 2 Diabetes often have a different composition of gut bacteria compared to those with normal glucose metabolism. Addressing gut health through lifestyle changes, such as eating more fiber-rich foods and fermented products, can thus be a pivotal strategy for improving insulin sensitivity and reducing diabetes risk.

Unpacking the Environmental Triggers
Understanding the environmental triggers behind Type 2 diabetes can shed light on your health and lifestyle choices. Factors like diet, physical activity, exposure to toxins, and stress play significant roles in metabolism and overall well-being. By recognizing these influences, you can begin to strategize actionable approaches that enhance your health and, potentially, ward off diabetes.
Modern lifestyle influences: Sedentary habits and stress
Today’s sedentary lifestyle, coupled with heightened stress levels, forms a perilous duo. Prolonged sitting not only impacts your metabolic rate but also increases insulin resistance, making it harder for your body to manage blood sugars effectively. Stress exacerbates this issue by elevating cortisol levels, a hormone linked to increased appetite and fat storage, which can worsen blood sugar control and lead to the onset of Type 2 diabetes.
Chemical exposure and its correlation with diabetes risk
The connection between chemical exposure and diabetes risk is increasingly evident, with studies highlighting various endocrine disruptors as culprits. Compounds like bisphenol A (BPA) and phthalates found in many plastics have been shown to interfere with insulin signaling and increase fat cell growth, which can accelerate the development of insulin resistance and Type 2 diabetes. Evidence suggests that even low-level exposure over time accumulates, raising your risk significantly. According to research, individuals with higher levels of these chemicals in their urine tend to show greater insulin resistance, indicating a direct correlation that poses serious health implications.
Rethinking Treatments and Preventative Strategies
Approaching Type 2 diabetes requires a shift in perspective on both treatment and prevention. Instead of solely relying on medications, you can explore integrated strategies that target the underlying causes. By embracing a holistic view of health, you can empower yourself to make informed choices that prevent the onset of diabetes and improve overall well-being.
Dietary interventions and their effectiveness
Your food choices play a key role in managing insulin sensitivity and blood sugar levels. Emerging evidence suggests that specific dietary interventions, such as a low-carbohydrate diet or a Mediterranean-style diet, can lead to significant improvements in metabolic health. These diets prioritize whole foods and healthy fats, which have been shown to positively impact glucose control and weight management.
Exercise and lifestyle modifications: Evidence-based approaches
Adopting regular physical activity is imperative in improving insulin sensitivity and reducing body fat. Research indicates that engaging in moderate exercise for just 150 minutes per week can greatly enhance your metabolic functioning. Additionally, incorporating strength training into your routine has been shown to increase your muscle mass, further aiding blood sugar regulation.
Evidence underscores that a consistent exercise regimen—whether it’s brisk walking, cycling, or yoga—can lead to profound benefits. A meta-analysis of multiple studies revealed that individuals who engage in lifestyle modifications, including a combination of aerobic and resistance training, experience a 30-50% reduction in their risk of developing Type 2 diabetes. Moreover, small changes like taking the stairs or integrating stretching into your daily routine can accumulate to create a significant impact on your health. These lifestyle changes foster a proactive approach, shifting the narrative from managing symptoms to preventing disease altogether.
Final Words
Hence, understanding that your pancreas isn’t inherently broken shifts the focus from blaming an organ to addressing lifestyle factors that contribute to Type 2 diabetes. By recognizing the role of diet, physical activity, and overall health, you can take proactive steps to manage your wellbeing. By making informed choices and prioritizing your health, you empower yourself to reverse the condition and improve your quality of life.
FAQ
Q: What are the primary factors that lead to Type 2 Diabetes if it’s not a broken pancreas?
A: Type 2 Diabetes is primarily influenced by lifestyle factors such as poor diet, physical inactivity, and obesity. These factors contribute to insulin resistance, where the body’s cells don’t respond well to insulin, leading to higher blood sugar levels. Furthermore, genetic predisposition, hormonal imbalances, and environmental factors can also play significant roles. Understanding these underlying causes can lead to more effective prevention and management strategies.
Q: How does insulin resistance develop in individuals with Type 2 Diabetes?
A: Insulin resistance develops when the body’s muscle, fat, and liver cells become less responsive to insulin, which is the hormone responsible for allowing glucose to enter cells for energy. This condition is often triggered by excess body fat, particularly around the abdomen, and can be compounded by a sedentary lifestyle and high-sugar or high-fat diets. Over time, this resistance can elevate blood sugar levels, resulting in the diagnosis of Type 2 Diabetes while the pancreas may still produce insulin, albeit not effectively utilized by the body.
Q: What lifestyle changes can help manage or reverse Type 2 Diabetes without deeming the pancreas ineffective?
A: Managing or potentially reversing Type 2 Diabetes can often be achieved through several lifestyle changes. These include adopting a balanced diet rich in whole foods, such as fruits, vegetables, lean proteins, and whole grains while reducing processed food intake. Regular physical activity, including both aerobic and strength-training exercises, is beneficial for improving insulin sensitivity. Additionally, maintaining a healthy weight and managing stress levels are important for overall metabolic health. In many cases, these changes can lead to significant improvements in blood sugar control and overall well-being.